Genomics and Psychiatric Disorders
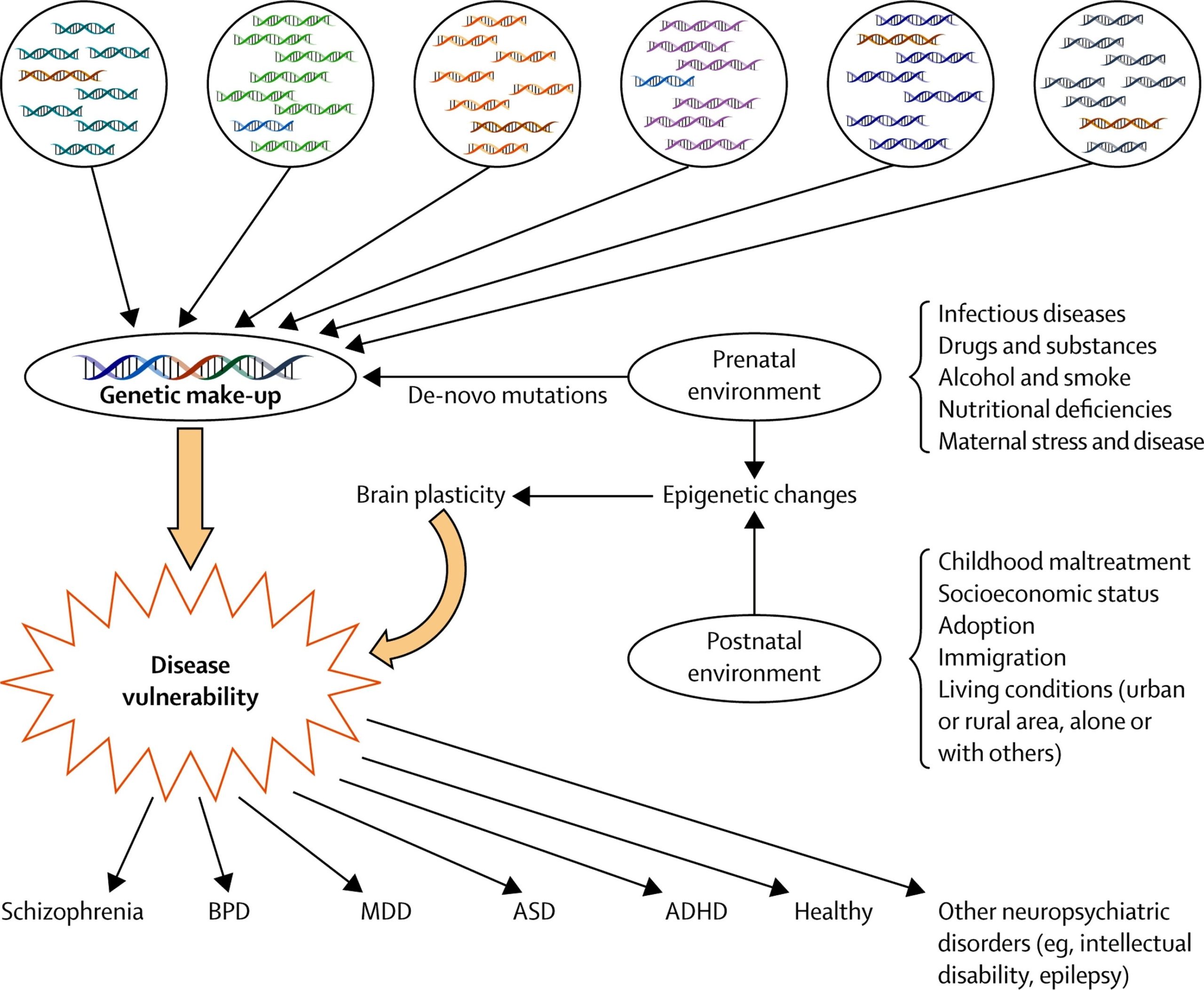
Psychiatric disorders, such as schizophrenia, bipolar disorder, major depressive disorder, attention-deficit/hyperactivity disorder (ADHD), and autism spectrum disorder (ASD), are common and result in significant morbidity and mortality. These disorders, although currently classified into distinct categories, show clinical overlap and familial co-aggregation, and share genetic risk factors.
Genomic Insights
Recent advances in psychiatric genomics have provided insight into the potential mechanisms underlying the overlap between these disorders, implicating genes involved in neurodevelopment, synaptic plasticity, learning, and memory. The emerging genetic architecture implies a large number of contributing loci and suggests that genetic risk of psychiatric disorders involves the combined effects of many common variants of small effect, as well as rare and de novo variants of large effect.
Genome-Wide Approaches
Recent genetic studies of psychiatric disorders have generally adopted one of the following genome-wide approaches:
1. Genome-Wide Association Studies (GWAS): These studies compare the frequencies of single-nucleotide polymorphisms (SNPs) between cases and controls. GWAS do not usually identify causal mutations, but instead identify SNPs in high linkage disequilibrium with the risk variant, thus highlighting genomic regions containing common risk alleles.
2. Rare Copy Number Variant (CNV) Studies: These studies identify sub-microscopic deletions and duplications of DNA associated with traits or diseases.
Impact of Genomics on Psychiatry
The highly polygenic and pleiotropic nature of psychiatric genetics will impact attempts to use genomic data for prediction and risk stratification, and also poses substantial challenges for conventional approaches to gaining biological insights from genetic findings. While there are many challenges to overcome, genomics is building an empirical platform upon which psychiatry can now progress towards better understanding of disease mechanisms, better treatments, and better ways of targeting treatments to the patients most likely to benefit.
Conclusion
The integration of genomics into psychiatry is paving the way for precision psychiatry, where healthcare is tailored more closely to the needs of individual patients. This requires progress in two areas: the development of more precise treatments and the ability to identify patients or groups of patients in the clinic for whom such treatments are likely to be the most effective. There is widespread optimism that advances in genomics will facilitate both of these endeavors.