Antifungal Medicines: Unveiling the Battle Against Fungal Infections
Fungi, those enigmatic organisms, inhabit diverse environments across the globe. While most fungi coexist peacefully with humans, some species wield the power to invade our bodies, causing infections. Enter antifungal medicines, the unsung heroes in our fight against these microscopic adversaries.
## Understanding Antifungal Drugs
Antifungal drugs are our allies in combating fungal infections. These medications serve a crucial purpose: they either kill fungal cells outright or inhibit their growth. But how do they achieve this delicate balance between eradicating fungi and sparing our own cells?
### 1. Targeting Fungal Structures
Antifungal drugs are like precision-guided missiles. They zero in on structures or functions vital to fungal cells but not essential for human cells. Two key targets are the fungal cell membrane and the fungal cell wall:
– Fungal Cell Membrane: Imagine the fungal cell as a tiny fortress surrounded by a protective membrane. Antifungal drugs disrupt this membrane, rendering it unstable. As leaks develop, the fungal cell faces imminent demise.
– Fungal Cell Wall: Another line of defense for fungi is their cell wall. Antifungal drugs make this wall more porous, weakening it. The result? Fungal cells become prone to bursting.
### 2. The Diverse Arsenal of Antifungal Drugs
Let’s delve into the pharmacological arsenal at our disposal:
#### Azoles
– Mechanism: Azoles interfere with an enzyme crucial for creating the fungal cell membrane. By destabilizing the membrane, they induce cell death.
– Subgroups:
– Imidazoles: Examples include:
– Ketoconazole: Effective against skin and hair infections, Candida skin and mucous membrane infections, blastomycosis, and histoplasmosis.
– Clotrimazole: Used for skin and mucous membrane infections.
– Miconazole: Effective against skin and mucous membrane infections.
– Triazoles: Examples include:
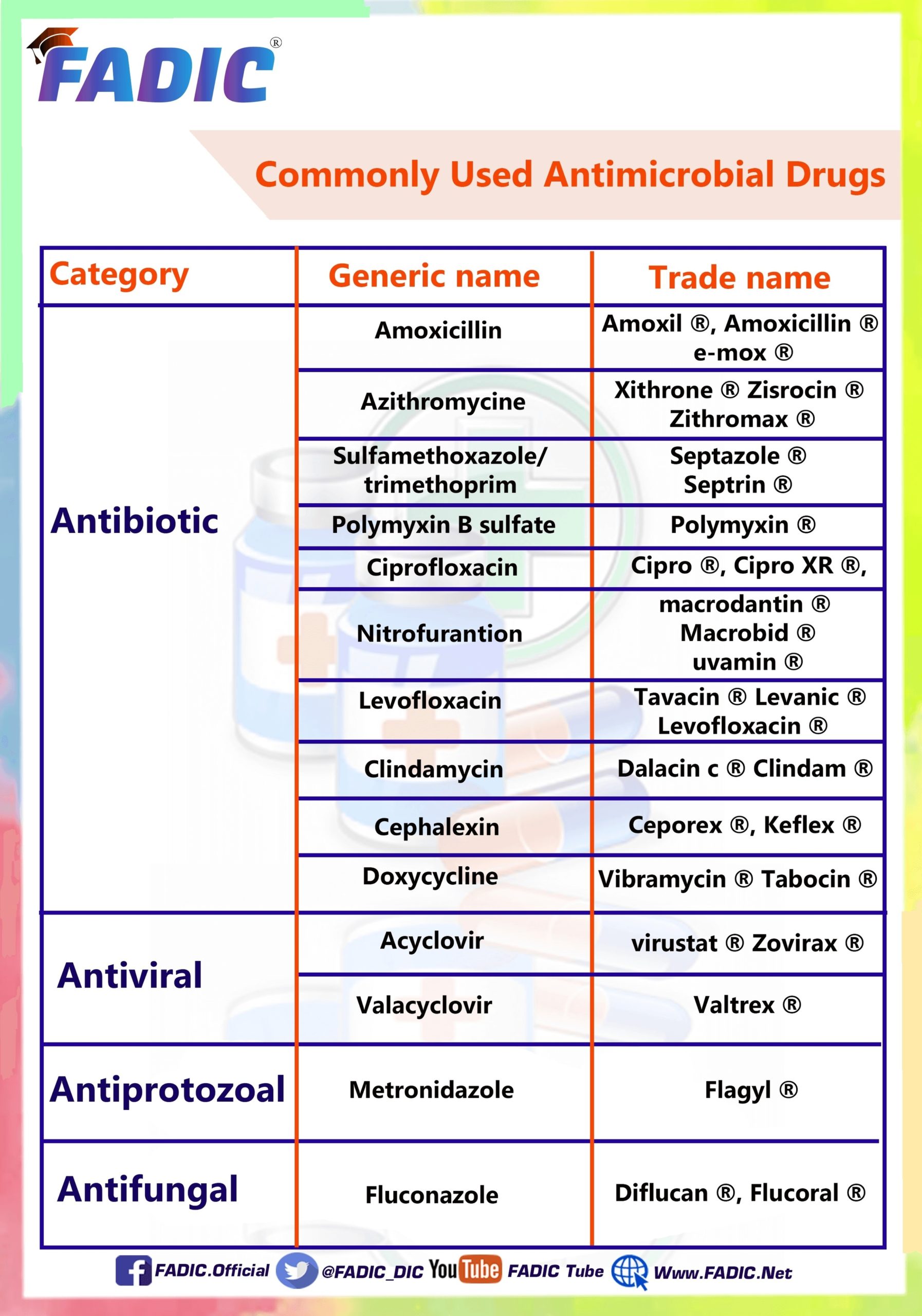
– Fluconazole: Treats various Candida infections (mucosal, systemic, and invasive) and cryptococcosis.
– Itraconazole: Battles aspergillosis, blastomycosis, histoplasmosis, mucosal Candida infections, and onychomycosis.
– Posaconazole: Used for aspergillosis (off-label), mucosal and invasive Candida infections.
– Voriconazole: Effective against aspergillosis and Candida infections.
– Isavuconazole: Targets aspergillosis and mucormycosis.
#### Polyenes
– Mode of Action: Polyenes render the fungal cell wall porous, making it susceptible to rupture.
– Applications:
– Amphotericin B: Used for systemic fungal infections, including cryptococcal meningitis.
– Echinocandins (anidulafungin, caspofungin, micafungin): Effective against various fungal infections.
– Flucytosine: Aids in fungal treatment.
### 3. Administration Routes
Antifungal drugs come in different forms:
– Oral: Taken by mouth.
– Topical: Applied directly to the skin or mucous membranes.
– Intravenous (IV): Administered directly into the bloodstream.
### 4. When to Seek Help
While mild fungal infections may resolve with over-the-counter treatments, serious or persistent cases demand professional attention. If symptoms persist or worsen, consult a healthcare provider promptly.
### 5. Prevention and Caution
Preventing fungal infections involves maintaining good hygiene, avoiding damp environments, and minimizing risk factors. Remember, antifungal medicines are our allies, safeguarding us from the unseen world of fungi.
In this battle, science wields its sword, and antifungal drugs stand as our silent guardians, ensuring that fungi remain mere shadows in our lives. ?????
: [Healthline](https://www.healthline.com/health/fungal-infection/antifungal)
: [Wikipedia](https://en.wikipedia.org/wiki/Antifungal)
: [Merck Manuals](https://www.merckmanuals.com/professional/infectious-diseases/fungi/antifungal-medications).
o